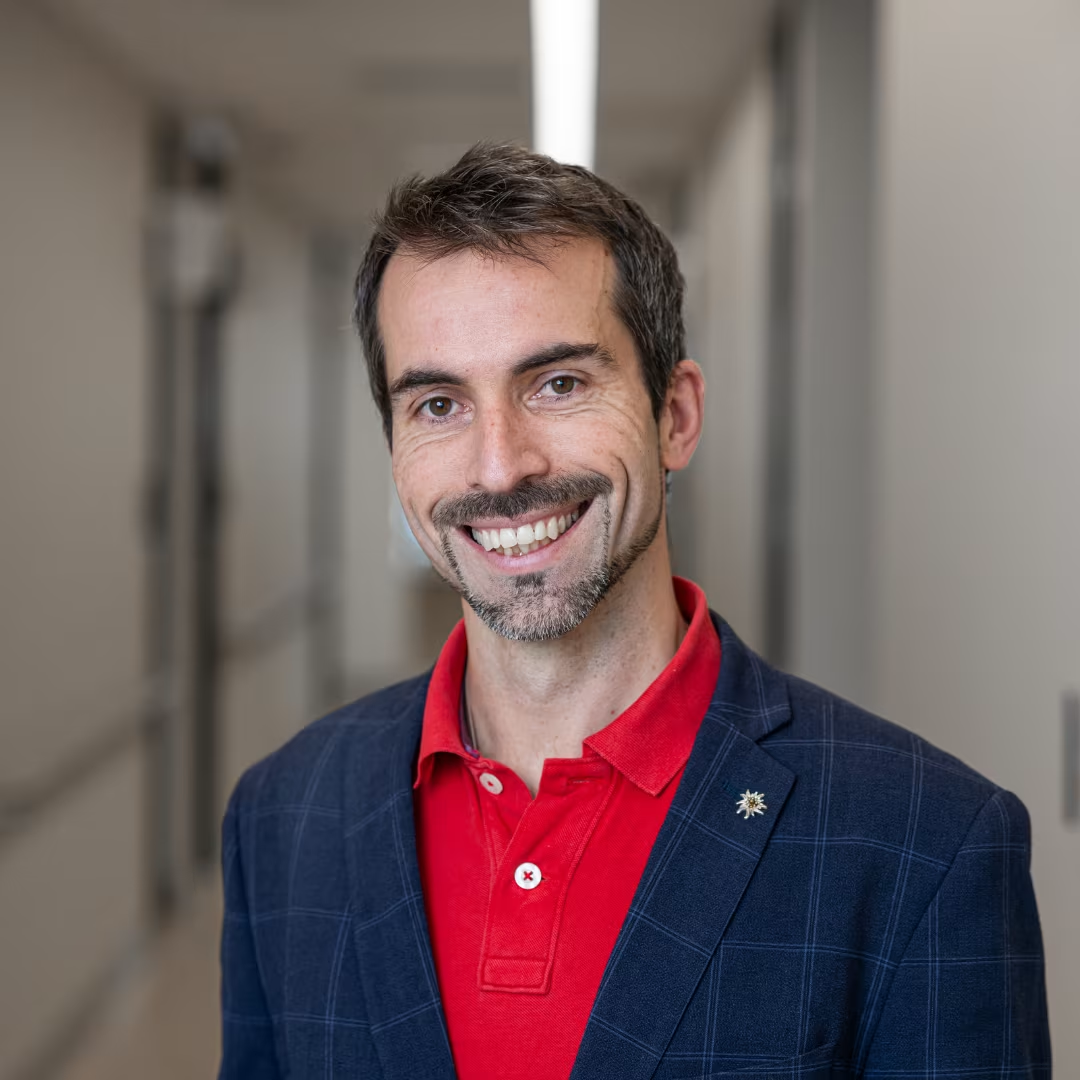
Standardized Definition of Progression Independent of Relapse Activity (PIRA) in Relapsing-Remitting Multiple Sclerosis.
Description:Progression independent of relapse activity (PIRA) is a significant contributor to long-term disability accumulation in relapsing-remitting multiple sclerosis (MS). Prior studies have used varying PIRA definitions, hampering the comparability of study results. To compare various definitions of PIRA. This cohort study involved a retrospective analysis of prospectively collected data from the MSBase registry from July 2004 to July 2023. The participants were patients with MS from 186 centers across 43 countries who had clinically definite relapsing-remitting MS, a complete minimal dataset, and 3 or more documented Expanded Disability Status Scale (EDSS) assessments. Three-hundred sixty definitions of PIRA as combinations of the following criteria: baseline disability (fixed baseline with re-baselining after PIRA, or plus re-baselining after relapses, or plus re-baselining after improvements), minimum confirmation period (6, 12, or 24 months), confirmation magnitude (EDSS score at/above worsening score or at/above threshold compared with baseline), freedom from relapse at EDSS score worsening (90 days prior, 90 days prior and 30 days after, 180 days prior and after, since previous EDSS assessment, or since baseline), and freedom from relapse at confirmation (30 days prior, 90 days prior, 30 days before and after, or between worsening and confirmation). For each definition, we quantified PIRA incidence and persistence (ie, absence of a 3-month confirmed EDSS improvement over ≥5 years). Among 87 239 patients with MS, 33 303 patients fulfilled the inclusion criteria; 24 152 (72.5%) were female and 9151 (27.5%) were male. At the first visits, the mean (SD) age was 36.4 (10.9) years; 28 052 patients (84.2%) had relapsing-remitting MS, and the median (IQR) EDSS score was 2.0 (1.0-3.0). Participants had a mean (SD) 15.1 (11.9) visits over 8.9 (5.2) years. PIRA incidence ranged from 0.141 to 0.658 events per decade and persistence from 0.753 to 0.919, depending on the definition. In particular, the baseline and confirmation period influenced PIRA detection. The following definition yielded balanced incidence and persistence: a significant disability worsening compared with a baseline (reset after each PIRA event, relapse, and EDSS score improvement), in absence of relapses since the last EDSS assessment, confirmed with EDSS scores (not preceded by relapses within 30 days) that remained above the worsening threshold for at least 12 months. Incidence and persistence of PIRA are determined by the definition used. The proposed standardized definition aims to enhance comparability among studies.